In my previous blog, the concept of cost-effectiveness in cancer care was discussed. However, one needs to step back in order to understand the value proposition of cancer care: who benefits most, society as a whole or the individual? It’s also important to understand what should be measured: improved quality of life or length of life? Then come the cost issues surrounding cancer care. Who pays for it and how much do they pay?
Let’s first discuss cost. According to the National Cancer Institute, the annual direct cost for cancer care in the U.S. was $125 billion in 2010, and is projected to grow to $173 billion by 2020.
Market distortions that commonly exist in drug cancer care, which do not exist in a competitive and efficient market, drive pricing upward. First, monopolistic pricing is created when a drug company receives a patent for the cancer therapy. There is also inelastic demand for the therapy—one likely needs it to survive. What’s more, coverage of drugs such as chemotherapeutics is dictated by law, requiring Medicare to pay for it. Lastly, there is significant lobbying and support for cancer care from cancer nonprofit organizations, with more than 250 in existence across the U.S. These nonprofits can create negative publicity when denial of cancer care is issued by an insurer.
These distortions help create relatively higher costs and “protected” pricing in cancer care that does not exist with other therapies. They also incentivize drug companies to develop marginally effective treatments.
The question becomes: How does one then address these high-cost issues?
One way could be to increase the use of comparative effectiveness analysis, which can help align resource use with its intended benefit. The medical community can use these types of analyses to refuse the use of new drugs that are more expensive than other drugs without demonstrated improved outcomes, such as better quality of life, longer life and fewer side effects.
Another strategy involves changing the practice patterns of physicians in certain situations. Examples of this include:
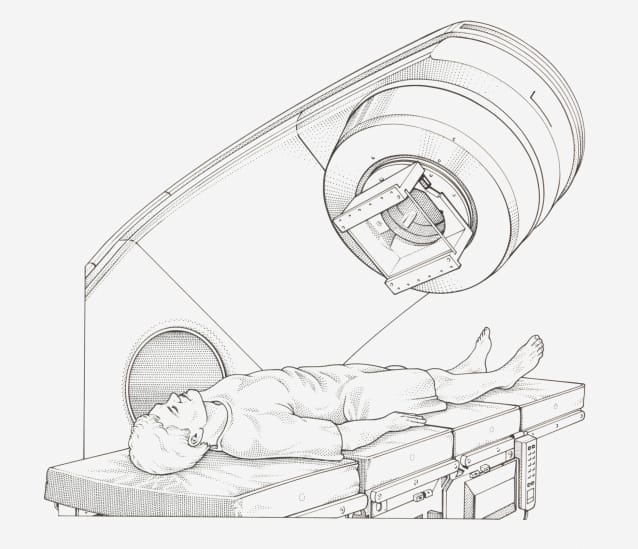
• Limiting chemotherapy to clinical trials for patients that do not respond to three consecutive regimens
• Limiting chemotherapy to patients with good performance status or patients able to walk unaided into the clinic to receive chemotherapy. The implementation of such a threshold could decrease the use of chemotherapy at the end of life.
• Ensuring in all circumstances that the cancer treatment is used for its intended purpose. In the past, oncologists have had flexibility in selecting treatments for patients.
Once we tackle these issues of high cost, we can then examine the issues of benefits to the community and to patients, which we will do in my next blog post.
Editor’s note: Read Jeff’s previous submission, “Cutting the Waste in the Cancer Chase,” for an introduction to this topic.