One of the issues in health care is unnecessary care provided to patients based on inaccurate diagnostic test results.
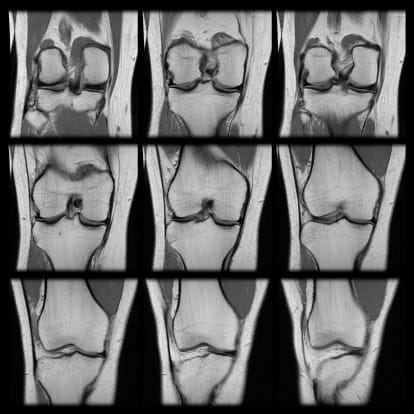
My colleagues and I recently published a paper in BMC Health Services Research on the use of MRI diagnostic testing versus a needle arthroscope for evaluating damage and pathology to large joints such as the knee. In patients with very deep-seated pathology such as meniscal tears (cartilage padding on the surface of the tibia that comes into contact with the femur), MRI findings are not accurate. There are a significant number of patients, approximately 20 percent, where the MRI shows pathology or damage when in fact there is none. In many cases, these false positives go on to surgical arthroscopy. An alarming statistic is that in 99 percent of arthroscopy cases, there is something done surgically to the patient.
With such a high false positive rate—20 percent—there should be significantly less of these surgical cases being performed. The finding in our paper was that approximately $400 million annually may be spent on unnecessary care to large joints.
And unnecessary care by definition is substandard care.
Recent studies published in the New England Journal of Medicine by Jeffrey N. Katz in May 2013 and Raine Sihvonen in December 2013 demonstrated that there was no clinical benefit to meniscus repair when performed against a sham or fake procedure versus physical therapy.
That begs the question, why are these procedures being done? There are several explanations. Physicians may be concerned about legal issues and may do the procedure to placate the patient. Physicians want to help patients and may do the procedure with the hope that their knee pain will improve. Or there is the perverse financial incentive built into the health care payment system that rewards volume over value; do a procedure and get paid for the procedure regardless of the outcome.
Recent advances in diagnostics may assist in lowering this false positive rate and reducing unnecessary surgical arthroscopic procedures. Our recent paper showed that products like the Visionscope Imaging System (VSI), a small-bore arthroscopic imaging device the size of a hypodermic needle, used under local anesthesia in the physician office setting versus in a more costly hospital operating room, significantly reduces the false positive rate and can significantly reduce follow-on surgical procedures. VSI can identify meniscal lesions accurately and allow a clinician to determine if surgical repair of meniscal damage, present or not, is really needed.
Such devices might make care more appropriate, reduce the need for unnecessary care and make our entire health care system more cost-efficient.
Editor’s note: For full disclosure, Jeff works as a reimbursement consultant for Visionscope.