There is an urban myth circulating in some corners of the University of Pennsylvania that suggests AcademyHealth, the country’s largest organization of health service researchers, was originally created at the Leonard Davis Institute of Health Economics (LDI). That isn’t exactly true at the same time it’s not totally wrong. There was significant involvement and now, as LDI celebrates its 50th anniversary, it seems an appropriate time to tell that story.

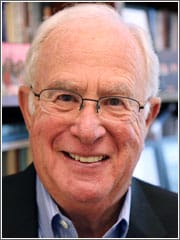
Photo: Will Dickey, 2016. In 1981, Wharton School Professor and LDI Executive Director William Pierskalla was a founding officer of the organization that went on to become today’s AcademyHealth.
Both LDI and its Executive Director from 1978 to 1983—William Pierskalla—played important roles in the series of events that resulted in the creation of the organization that is now a leading power in the world of health care delivery research.
Details of the story come from interviews with participants as well as the archives of LDI and AcademyHealth. It begins in the 1960s when both the new federal Medicare and Medicaid programs and the modern field of academic health services research were symbiotically emerging together.
The players are health services research pioneers Clifton Gaus, Stuart Altman, William Pierskalla, Robert Blendon and a handful of other scientists who ultimately turned personal frustration into action that forever changed and energized their profession.
In 1967, as 19.5 million people enrolled in the Medicare program’s second year and overall national health care expenditures increased by 11.9 percent over the previous year, the LBJ White House ordered the Department of Health, Education and Welfare (HEW) to create a new National Center for Health Services Research and Development (NCHSRD).
Beyond Traditional Methods
HEW Secretary Wilbur Cohen announced that “providers of health services now face demands that exceed the capacity of traditional ideas, methods and institutions. We must seek answers, and find ways to contain the rapid rise of medical care costs. We must clearly identify the elements of health services, understand what they contribute to health and select the critical points at which well-designed experiments will result in more effective medical treatment, greater efficiency and greater availability of services to all our people.”

Former federal health care official Clifton Gaus’ early vision and tenacious organizational activities were the central, driving force that led to the creation of the AHSR.
The move was a boon to the country’s small and scattered group of health services research scientists who had only convened their first casual gathering six years earlier. Most of them, like Clifton Gaus, were connected to a rapidly expanding flock of health care-related federal agencies. Gaus was a newly-minted ScD out of Johns Hopkins who had studied under Kerr White, MD, the founding chair of Hopkins’ Department of Health Policy and Management.
An epidemiologist, White is credited with coining the term “health services research” to describe the science of studying how health care delivery is organized, financed, managed and evaluated. Nationally renowned as a pioneer in the field, White also chaired the HEW Secretary’s advisory committee that recommended and established that agency’s National Center for Health Services Research and Development (NCHSRD).
As an undergraduate and protégé of Professor White, Gaus went to Washington as a staffer on a White House research project evaluating HEW’s policy analysis capability. In 1972 Gaus was hired as an official in HEW’s new Office of Policy Analysis and there, worked closely with then-HEW Deputy Secretary for Planning and Evaluation, Stuart Altman, PhD, another health services research pioneer.
A Small Circle
During the next seven years, Gaus was heavily involved in health services research projects and helped organize the new Health Care Financing Administration (HCFA), where he became Associate Administrator for Policy Research. He and a small circle of colleagues including Altman and Philip Lee, a former HEW Assistant Secretary for Health and Scientific Affairs, spoke often about the the need for an independent national organization that could be the voice and advocate for health services research.
“From the earliest days that I knew him,” remembered Altman, “Clif was making the case that ‘if we don’t do something and become a lobbying force we will never get adequate funding’—he’d say ‘we couldn’t just sit back and think because we’re doing good things, the rest will come on its own; it won’t.’”
When initially created in 1968 with the enthusiastic support of the White House, HEW and Congress, the NCHSRD was generously funded. Meanwhile, increasing numbers of health services researchers were becoming an integral part of federal government management agencies. Still benefiting from the mutual embrace of health services research by the White House, HEW and Congress, the NCHSRD in 1977 launched five university-based national health services research centers. Four focused on various health policy issues. The other and most heavily funded—the National Health Care Management Center (NHCMC)—was established within the University of Pennsylvania’s Leonard Davis Institute of Health Economics (LDI); William Pierskalla was Director of both LDI and the NHCMC.
Along with Gaus, former HEW official Stuart Altman played a key role in the organization and founding of the AHSR.
Increasingly Complicated Relationships
As it often does, the happy alignment of Administration, Agency and Congressional agendas waned. Throughout the late 1970s, health services research lost fiscal traction in Congress as the relationship between researchers, government agencies and policymakers became increasingly complicated and frayed.
In his history of that era, Eli Ginsberg, PhD, a professor of economics at Columbia University, wrote there were “tools and techniques available that enable health services research to analyze various facets of the changing health care sector and in the process to illuminate hitherto unrecognized or misunderstood relationships and to put forward improved formulations. But when it comes to the policy arena, scholarship and analytical work take one only as far as the threshold, where an array of interest blocs, competing politicians, the media and still other potent groups are likely to be engaged participants.”
Sankey Williams, MD, who became an LDI Senior Fellow back in 1975 when he was a Penn RWJF Clinical Scholar, remembers that period when the power of health services research was just beginning to become apparent to health care’s major players.
“It was a new field of research that largely asked the question, ‘How do we make this system more efficient? What does efficiency mean in this context?’,” said Williams, who is a Professor of both Medicine and Health Care Management at Penn’s Perelman and Wharton Schools.
Political Backlash
“What it meant, people were realizing,” he continued, “is that if you’re getting overpaid, we’re going to generate data that shows you shouldn’t be overpaid. And lots of people in this industry are overpaid: the drug companies, the proceduralists, the hospitals. So, health services research was showing itself to be all about making sure these guys got less money. Guess how they and their Washington lobbyists responded?”
Beyond the issue of intensifying political backlash, government health services researchers were also grappling with internal struggles as one faction of top HEW officials wanted to continue funding academic research centers while another wanted to bring all health services research funding back inside the agency.
“During the last three years of the program, the other center directors and I had to fight each year to keep the funding because the then-NCHSRD director didn’t like the idea of having to pay out all this money on stuff he couldn’t control,” William Pierskalla remembered.
“This was something we were always talking about in the annual meetings of the center directors—how to keep the centers going,” Pierskalla continued. “And if we didn’t organize in some way that could make Congress better understand what health services research really did, we weren’t going to get very far.”

A senior vice president at the Robert Wood Johnson Foundation and member of the National Advisory Council of the Leonard Davis Institute of Health Economics, Robert Blendon in 1981 provided the funding for the feasibility study that laid the groundwork for the creation of the AHSR.
In 1979, tired of the bureaucratic tangles and political barriers that now confronted health services researchers within the government, Gaus left his HEW post and joined Georgetown University where he organized the Georgetown Health Policy Studies Center.
“Lack of Advocacy”
“I had strong feelings about how the NCHSRD was being run and its lack of a funding base and advocacy,” said Gaus, who is now CEO of the National Association of Accountable Care Organizations. “The bottom line was I didn’t think the research committee was having much of an input into the policy making at HEW at the time. And they were going to terminate the research centers program that I felt was quite important.”
The same discontent kept Gaus in ongoing discussions with Altman, Lee and a handful of other colleagues about how best to form, launch and grow a professional organization for health services researchers outside of government.
“I think we all recognized the need to elevate the perceived importance and standing of health services research,” said Gaus. “The thought was that the bigger the name, the higher the status, the broader the mandate, all increased the likelihood that we would prevail in budget battles and be able to have science influence the course of policy.”
Grant for Feasibility Study
Gaus also had a close ally in Robert Blendon, ScD, a long-time friend and former classmate at Hopkins. In 1980, Blendon was the Robert Wood Johnson Foundation Senior Vice President administering the funding of the new Georgetown Center. He provided the Center with an additional $25,000 (about $70,000 in 2016 dollars) to underwrite a feasibility study for the creation of an organization to be called the Association for Health Services Research (AHSR).
“There was a lot of debate about the idea at the time,” explained Blendon, who is now a Professor and Associate Dean at the Harvard T.H. Chan School of Public Health. “It was not a disagreement over whether or not this new field of research should grow; there was quite a consensus that it should. The issue was if it should be incorporated into an existing health organization rather than be a new and separate thing.”
“I shared Clif’s view that, in the long term, incorporation into existing organizations would not be ideal,” said Blendon. “A number of the potential organizations were not interdisciplinary. Or they were not focused on policy, or they had their own political agendas. So, in the end, the only funder Clif could convince about the need for a new Washington-based association was me.”
In that same period, LDI’s National Center for Health Care Management and the four other NCHSRD research centers were notified that their program grants would not be renewed and that the last annual meeting of those centers’ managers would be scheduled for January 1981 at Penn’s Leonard Davis Institute.
HSR’s Top Leaders
Because those centers were run and staffed by the country’s top echelon of health services research leaders, Gaus viewed the upcoming gathering as a unique opportunity.
“That’s when I reached out to LDI and Bill Pierskalla,” Gaus remembered. “The small group of us who were discussing the feasibility of a national organization saw the centers’ meeting at LDI as a way to get large scale buy-in to the idea.”
In November of 1980, as Pierskalla and his staff began organizing that two-day January 1981 meeting, he wrote invitation letters to more than three dozen NCHSRD directors and other top health services researchers around the country. He said the meeting’s purpose was to “focus on the future.”
On January 14 and 15, 1981, 39 attendees assembled in the fourth-floor conference room of LDI’s Colonial Penn Center building on Penn’s campus. There, Gaus led the discussion of both how an organization of health services researchers could potentially lobby “Congress, HHS, OMB, foundations and states,” and the pros and cons of various ways that organization could be structured. The three options discussed were informal network, association and legal corporation.
“That meeting was a phenomenal success,” Pierskalla remembered. “The attendance was great and it was two days of very interesting talk and people interacting and some of those people—like Gaus and Altman—were really well connected in Washington and had a lot of ideas about how we could take it forward on the political side. Gaus was the driving force of the association idea.”
Consensus to Organize National HSR Association
The 42-page LDI after-report of that meeting notes the event “concluded with group consensus to proceed with organizing an association of health services researchers which would have as its primary purposes: to increase awareness of and appreciation for health services research, to provide a focal point in the field for health services research activity and to participate in decisions at the federal level that affect the health services research field.”
The level of excitement generated at the LDI gathering is evident in the January 19 letter in which attendee Edward Hughes, MD, MPH, of Northwestern University thanked Pierskalla for organizing the meeting and told him, “I am looking forward very much to some good collective action coming out of our ‘Association’—and some fun too!”
Less than three months later, Gaus of Georgetown, Altman of Brandeis, Pierskalla of Penn LDI, Hughes of Northwestern, and Lee of the University of California, San Francisco, gathered at Georgetown to legally create that association. Gaus had brought in two attorneys to prepare and execute the legal papers for two separate entities: the Association for Health Services Research (AHSR) and the Foundation for Health Services Research (FHSR). The latter was solely focused on fundraising. According to Gaus, who was AHSR founding President, he and the four other new officers of the organization each kicked in $5,000 to fund initial operations.
“Major Milestone”
Looking back, Gaus characterized the LDI-organized 1981 meeting as “clearly a major milestone in our efforts to launch AHSR.”
Pierskalla pointed out how fast the AHSR started to coalesce and grow after they hired one of Altman’s students from Brandeis, Alice Hersh, MS, to manage day-to-day operations in 1982. “She was an incredibly talented person.” Pierskalla remembered.
In June of 1984 when the AHSR held its first annual meeting with the theme of “Health Services Research and Public Policy” in Chicago, 350 people attended.
In 2000 the AHSR and the health policy analysis organization the Alpha Center merged to create AcademyHealth, which today routinely hosts nearly 3,000 attendees at its annual conferences.
Altman, who still attends those gatherings, noted that when he sits in an AcademyHealth plenary session held in a ballroom as large as a football field filled with a sea of people, he is overwhelmed by how far the AHSR idea has come.
“It’s just so impressive when you see the size of it today,” he said. “Sometimes I find myself saying, ‘My God! We started all this.’”
Hoag Levins is Editor of Digital Publications at the University of Pennsylvania’s Leonard Davis Institute of Health Economics (LDI) and a former reporter and editor at newspapers and magazines in Philadelphia, New York and Washington, D.C.
Editor’s note: This post was originally published by the Leonard Davis Institute of Health Economics as part of their eMagazine, the LDI Health Economist. View the original post here.