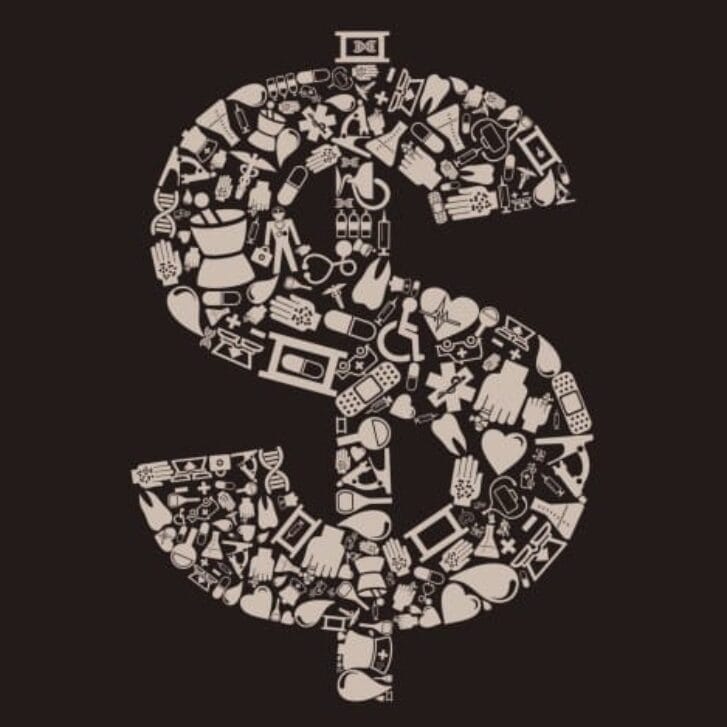
An op-ed article by Dr. Rita Redberg appeared in The New York Times back on May 25, 2011 related to Medicare’s paying for treatments with no known benefit, such as for kyphoplasty and vertebroplasty. In this article, the chief actuary for Medicare estimated that 15 to 30 percent of health care expenditures are wasteful suggesting that as much as $150 billion could be cut from the Medicare budget without reducing needed services. Back on October 24, 2008, Billy Beane, Newt Gingrich and John Kerry published a New York Times piece, “How to take American Health Care From Worst to First.” They suggested that smarter statistical analysis could lower the costs of the American health care system in a way similar to the “Moneyball” that Beane employed in making the Oakland Athletics a winning team in spite of having the lowest payroll in baseball.
Beane, Gingrich and Kerry mentioned one particular method of smarter statistical analysis, the Cochrane Collaboration, which involves systematic, evidence-based reviews of medical literature. In fact, applying Cochrane analytics allows us to challenge accepted medical practices and the inefficient allocation of resources.
Providers tend to choose more expensive technologies over less expensive versions even when the more expensive versions fail to demonstrate a better value or even a clear clinical benefit.
A perfect example is total knee implants. The U.S. market size for total knee implants exceeded 575,000 procedures in 2010 most of which were performed on Medicare-eligible patients. The average selling price for a metal-backed total knee implant is estimated at $5,450. Assuming that 55 percent of all total knee implants are performed on Medicare patients, Medicare spends $1.7 billion per year for total knee implants.
Recently, we performed a systematic review and meta-analysis of randomized controlled trials using the Cochrane methodology examining the use of a less expensive, polyethylene tibial implant. It costs roughly $1,600 less per implant. We found that the less-expensive component performed just as well as the more expensive versions on the outcomes of durability, function and adverse events over a 15-year period
Such meta-analyses can provide more precise estimates of the effects of an intervention than those derived from an individual study. These types of reviews are beginning to be used by payers and medical societies in establishing coverage determinations and in writing clinical guidelines.Despite the evidence above, the less expensive tibial components comprise only 1 percent of all U.S. knees implanted annually. If they were instead used in place of the more expensive metal-backed implants, Medicare could save greater than $500 million annually.
Why isn’t this product used more often? What can be done? We will discuss this in the next blog.
Editor’s note: The findings from Jeff’s study were published in the Journal of Bone and Joint Surgery (JBJS), the leading peer-reviewed orthopedic journal in the U.S. Read Part 2 of Jeff’s “Moneyball for Health Care” here.